Original story at U of U Health.
An international team of 18 researchers, including a scientist at University of Utah Health, have determined that the earliest cases of COVID-19 in humans arose at a wholesale fish market in Wuhan, China, in December 2019. They linked these cases to bats, foxes and other live mammals infected with the virus sold in the market either for consumption as meat or for their fur.
The finding, published in the July 26, 2022, issue of Science, aligns with early reports, later dismissed by senior Chinese officials, that live animals sold at the Huanan Seafood Wholesale Market were the likely source of the pandemic that has claimed at least 6.4 million lives since it first emerged in China nearly three years ago.
“These are the most compelling and most detailed studies of what happened in Wuhan in the earliest stages of what would become the COVID-19 pandemic,” says Stephen Goldstein, Ph.D., a co-author of the study led by senior author Kristian Anderson, Ph.D., from the Scripps Research Institute in La Jolla and first author Michael Worobey, Ph.D., from the University of Arizona. Goldstein is a postdoctoral scientist in the department of Human Genetics at U of U Health. “We have convincingly shown that the wild animal sales at the Huanan Market in Wuhan are implicated in the first human cases of the disease.”
Among the study’s key findings:
- The emergence of SARS-CoV-2, the virus that causes COVID-19, can likely be traced to one or more of the 10 to 15 stalls in the market that sold rats, porcupines, badgers, hares, foxes, hedgehogs, marmots, and Chinese muntjac (a small deer). Health officials and researchers detected SARS-CoV-2 on animal cages, carts, and drainage grates in these venues.
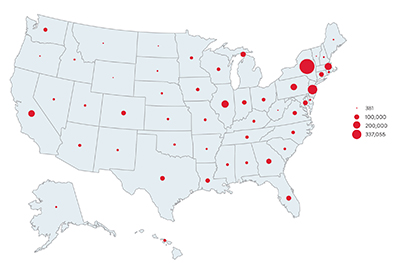
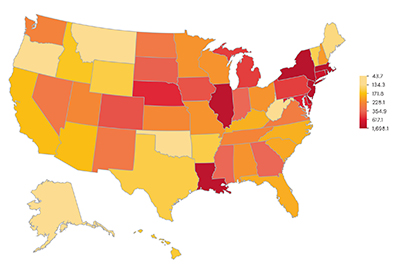
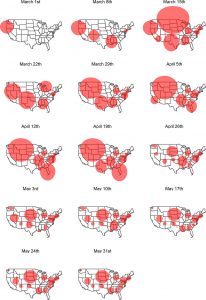
- The only areas where the virus was spreading in December 2019 were in neighborhoods within a half-mile of the market. Previously, some researchers had suggested that the virus was brought into the market from elsewhere in the city and spread among its patrons. Instead, the new findings strongly suggest that the virus originated in the market via live animal sales, and slowly spreading from there into nearby neighborhoods and then the city at large.
- Two variants of the SARS-CoV-2 virus were detected at the market. That suggests both variants originated independently at the market and helps confirm the researchers’ hypothesis that early spread of the infection began there. If the virus originated elsewhere, it’s more likely that only a single variant would have been found.
The researchers say that moving forward, public officials should seek better understanding of the wildlife trade in China and elsewhere and promote more comprehensive testing of live animals sold in markets to lower the risk of future pandemics.
In a press conference, Stephen Goldstein, PhD, explains and answers questions about the study.
####
The research published as “The Huanan Seafood Wholesale Market in Wuhan Was the Early Epicenter of the COVID-19 Pandemic” in Science on July 26, 2022.