In science as in life, the past 16 months have been nothing short of a crucible: “a situation of severe trial… leading to the creation of something new,” as the Oxford dictionary describes it. The pandemic charged in on a cloud of confusion that gave way to ingenuity, promising to forever change how research at the University of Utah is done.
Those early days proved critical for setting the U on a trajectory to make a difference. When COVID-19 shifted from threat to reality, scientists faced a difficult decision. Should we keep ourselves, co-workers, and their families safe by staying home? Or should science soldier on? After all, the one thing that would hasten the end of the pandemic is a set of science-based solutions to combat the virus and its endless impacts.
While research programs across the country quickly shut down, the U’s Office of the Vice President for Research (VPR) eliminated the dilemma by building a safe environment so researchers could continue their work. Personnel donned personal protection equipment, deployed sanitation stations, staggered work hours, and shrank their in-person workforce to an essential few. Just weeks after the first COVID-19 cases emerged in Utah, the Office of the VPR, in collaboration with the U’s Immunology, Inflammation, and Infectious Disease Initiative (3i), made another critical decision. They invested $1.3 million in seed funding to jump-start more than 55 COVID-19 research projects across campus.
(5 minute video) In a time of crisis, University of Utah researchers mobilized rapidly to meet the challenges of a global threat. Video credit: Charlie Ehlert
Today, the number of COVID-19 research projects at the U has swelled to more than 400, rooted in every discipline imaginable, from political science to engineering, medical research to health disparities, environmental science to business.
With a deep understanding of the immense importance and immediate need, investigators and administrators moved mountains to make COVID-19 research happen. They innovated and applied their knowledge in different ways. If their new work required resources that didn’t exist, they built them. If they needed additional expertise, they reached across campus—and out to the public and larger scientific community—to form collaborations. To share insights and resolve issues, 3i initiated regular, COVID-19-focused symposia, uniting scientists from across campus in a way that had not been done before.
“I’m humbled by how much our research community has stepped up to the plate,” says Andrew Weyrich, PhD, Vice President for Research. “Their collaborative spirit and values allowed us to overcome challenges throughout the pandemic.”
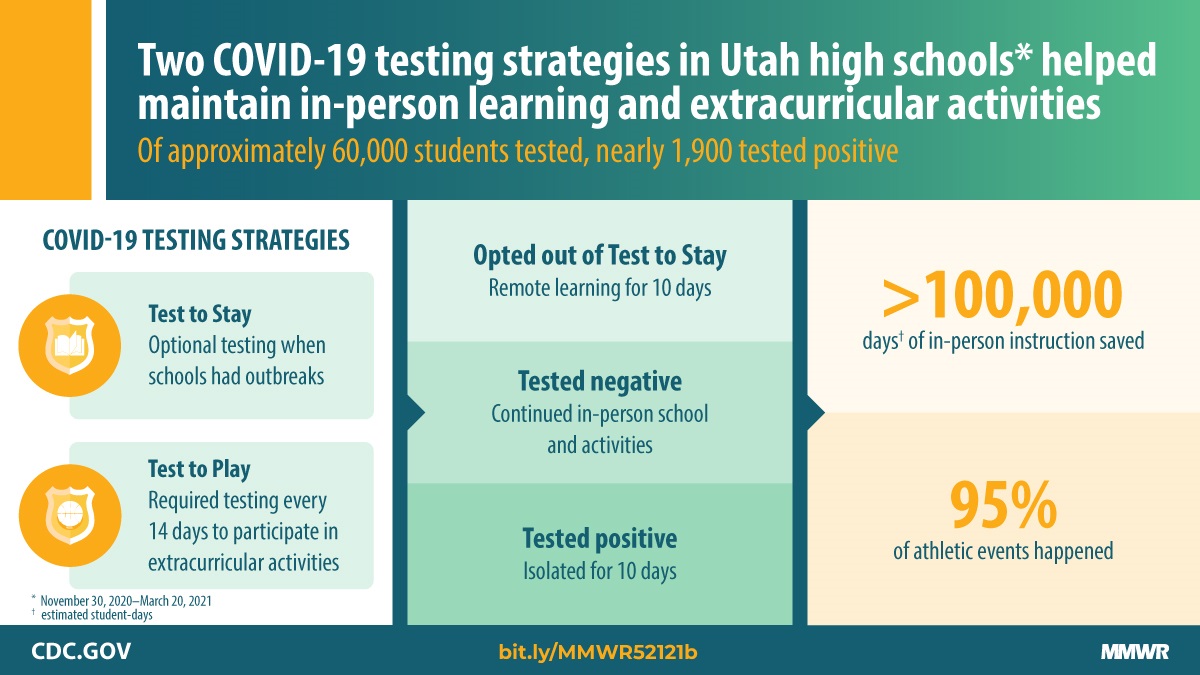
Beyond research, U scientists’ in-depth knowledge equipped them to serve as guiding voices for the public and policymakers. Media called on them to explain intricacies of the disease and its solutions, while state and national agencies consulted with them on strategies for protecting communities and forming evidence-based decisions.
(1 hour video) Seminar to the community about the U of U COVID-19 research response.
Data reveal truths, and the numbers from this time tell a story of impact. U investigators have published more than 200 COVID-19 scientific papers that have become resources for the global scientific community, and their expertise has been cited in more than 500 news stories. Government agencies and private foundations are also relying on the U, investing more than $62 million in U-led COVID-19 research. “University of Utah is on track for having one of the most comprehensive COVID-19 research programs in the country,” Weyrich says. As the fight against the pandemic and its long-lasting effects plays out over the years to come, these contributions will only continue to grow.
The world had never encountered a virus like this one, but the challenges it brought made an already robust research enterprise even stronger. Newly honed connections within and beyond the university mean that, moving forward, researchers can respond quickly and comprehensively to demands of the future, whatever they may be.
“The pandemic has taught us that when we work together, we can accomplish anything,” Weyrich says.