Changes in blood platelets triggered by COVID-19 could contribute to the onset of heart attacks, strokes and other serious complications in some patients who have the disease, according to University of Utah Health scientists. The researchers found that inflammatory proteins produced during infection significantly alter the function of platelets, making them “hyperactive” and more prone to form dangerous and potentially deadly blood clots.
They say better understanding the underlying causes of these changes could possibly lead to treatments that prevent them from happening in COVID-19 patients. Their report appears in Blood, an American Society of Hematology journal.
“Our finding adds an important piece to the jigsaw puzzle that we call COVID-19,” says Robert A. Campbell, senior author of the study and an assistant professor in the Department of Internal Medicine. “We found that inflammation and systemic changes, due to the infection, are influencing how platelets function, leading them to aggregate faster, which could explain why we are seeing increased numbers of blood clots in COVID patients.”

Depiction of a blood clot forming inside a blood vessel. 3D illustration
Emerging evidence suggests COVID-19 is associated with an increased risk of blood clotting, which can lead to cardiovascular problems and organ failure in some patients, particularly among those with underlying medical problems such as diabetes, obesity or high blood pressure.
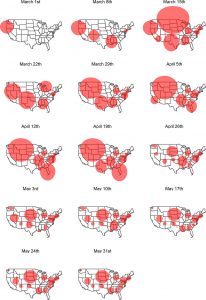
To find out what might be going on, the researchers studied 41 COVID-19 patients hospitalized at University of Utah Hospital in Salt Lake City. Seventeen of these patients were in the ICU, including nine who were on ventilators. They compared blood from these patients with samples taken from healthy individuals who were matched for age and sex.
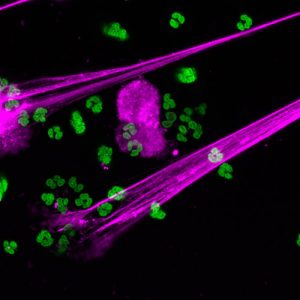
Using differential gene analysis, the researchers found that SARS-CoV-2, the virus that causes COVID-19, appears to trigger genetic changes in platelets. In laboratory studies, they studied platelet aggregation, an important component of blood clot formation, and observed COVID-19 platelets aggregated more readily. They also noted that these changes significantly altered how platelets interacted with the immune system, likely contributing to inflammation of the respiratory tract that may, in turn, result in more severe lung injury.
Surprisingly, Campbell and his colleagues didn’t detect evidence of the virus in the vast majority of platelets, suggesting that it could be promoting the genetic changes within these cells indirectly.
One possible mechanism is inflammation, according to Bhanu Kanth Manne, one of the study’s lead authors and a research associate with the University of Utah Molecular Medicine Program (U2M2). In theory, inflammation caused by COVID-19 could affect megakaryocytes, the cells that produce platelets. As a result, critical genetic alterations are passed down from megakaryocytes to the platelets, which, in turn, make them hyperactive.
In test-tube studies, the researchers found that pre-treating platelets from SARS-CoV-2 infected patients with aspirin did prevent this hyperactivity. These findings suggest aspirin may improve outcomes; however, this will need further study in clinical trials. For now, Campbell warns against using aspirin to treat COVID-19 unless recommended by your physician.
In the meantime, the researchers are beginning to look for other possible treatments.
“There are genetic processes that we can target that would prevent platelets from being changed,” Campbell says. “If we can figure out how COVID-19 is interacting with megakaryocytes or platelets, then we might be able to block that interaction and reduce someone’s risk of developing a blood clot.”
Find original post here.
This study titled, “Platelet Gene Expression and Function in COVID-19 Patients,” was funded by the National Institutes of Health, the University of Utah Health 3i Initiative and the American Heart Foundation.